Difference between revisions of "Insulin Resistance"
m (added bold to text) |
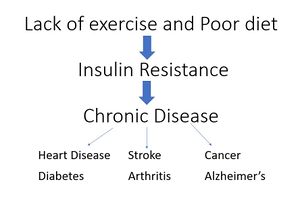
(added graphic insulin resistance leads to chronic disease) |
||
| Line 37: | Line 37: | ||
As many health issues have common roots originating from insulin resistance, this advice is good for all genetic populations, but especially for ApoE4s given the association with Alzheimer’s, cardiovascular disease, and lowered longevity. | As many health issues have common roots originating from insulin resistance, this advice is good for all genetic populations, but especially for ApoE4s given the association with Alzheimer’s, cardiovascular disease, and lowered longevity. | ||
[[File:Insulin resistance leads to chronic disease.JPG|thumbnail|Insulin Resistance leads to chronic disease]] | |||
=== Insulin Resistance's Link to Alzheimer’s disease === | === Insulin Resistance's Link to Alzheimer’s disease === | ||
Revision as of 19:26, 26 July 2017
Insulin Resistance is the root of many health concerns, particularly those that ApoE4s are susceptible to. A person can be insulin resistant without being Type 2 Diabetic, but Type 2 Diabetes by definition includes insulin resistance. There are many factors which can play in to insulin resistance, but a person is particularly vulnerable to developing insulin resistance if they are sedentary and eat a poor diet.
Introduction to Insulin Resistance and associated terms
Blood Sugar - the amount of glucose present in the blood. Blood Sugar Glucose is the body’s primary source of energy. The body works to keep blood glucose regulated to a near constant level (metabolic homeostasis). Foods that greatly interrupt this homeostasis by rapidly increasing blood sugar are called high glycemic. Foods that are high glycemic tend to be those containing sugar and carbohydrates, especially simple carbohydrates, although excess protein will also raise blood sugar levels (gluconeogenesis).
Insulin – A hormone made by the pancreas that allows the body to use or to store glucose. When stored, it becomes fat. Fat is stored in fat cells, called adipocytes. Insulin works to keep the blood sugar steady, neither too high too high (hyperglycemia) or too low (hypoglycemia).
Type 2 Diabetes -- A metabolic disorder characterized by high blood sugar, insulin resistance, and low insulin. Also referred to as T2D or Type 2 Diabetes mellitus. In T2D, the pancreas doesn’t produce sufficient insulin because either the insulin resistance is too high or the ability of the pancreas to produce a compensating amount of insulin (compensatory hyperinsulinemia) reaches a point where it drops. Unlike Type 1 Diabetes, T2D is largely preventable (often associated with obesity) and even reversible, seeReversing T2D start guide. T2D is preceded by pre-diabetes.
Pre-Diabetes – A period of many years when the blood sugar level is higher than normal but not yet high enough to be type 2 diabetes. Without diet and/or lifestyle intervention, pre-diabetes will become T2 diabetes. During this long phase, the blood glucose levels slowly rise and insulin resistance similarly rises, but the body produces enough insulin to overcome this resistance, so blood glucose remains relatively normal.
Insulin Resistance – When the body’s cells fail to respond normally to insulin, they become “resistant” to the insulin hormone, leading to high blood sugar. In turn, the beta cells of the pancreas increase their production of insulin, contributing to a high blood insulin level. A person can be insulin resistant without having T2D. With insulin resistance, the fat cells expand to a point where they can’t get any bigger (adipocyte hypertrophy), they don’t get enough oxygen, they create inflammation, and the fatty acids look for other storage places, so they go into the abdominal cavity (visceral fat), other organs (liver, pancreas, kidneys), and muscle.
Insulin Sensitivity – When the body responds quickly to the effects of insulin and requires smaller amounts of insulin to lower blood glucose levels. Generally speaking, having good sensitivity to insulin is a sign of good health.
Non-Alcoholic Fatty Liver Disease (NAFLD) – Also referred to as Non-Alcoholic Steatohepatitis (NASH). A condition when a liver accumulates fat not due to alcohol which leads to abnormalities in liver function. This occurs under conditions of persistent high insulin. A fatty liver can precede Type 2 diabetes. If the liver becomes fat it becomes insulin resistant, so it’s not regulated by insulin appropriately, therefore throughout the night the liver secretes more and more glucose. When people with fatty liver wake up in the morning they will have high glucose even though they haven’t eaten for 8-10 hours. When the liver tries to decompress itself from fat, it makes triglycerides through de novo lipogenesis. A person with high triglycerides, low HDL, and small dense LDLs is likely to have fatty liver even if they are a lean/normal weight person.
TOFI – Thin Outside, Fat Inside. These are people who have a limited ability to store fat. They look thin, have acceptable Body Mass Index (BMI) level, but since they have limited capacity to store fat they can be horribly insulin resistant or T2 diabetic. It’s been hypothesized that everyone has a Personal Fat Threshold (PFT). When that PFT is exceeded, the development of T2D us likely. See Normal weight individuals who develop type 2 diabetes: the personal fat threshold Conversely, there’s also a small percentage of obese people who, through a process called hyperplasia just develop additional adipocytes (fat cells), thereby not reaching a PFT or developing insulin resistance or T2D.
Hemoglobin A1c – More commonly referred to as HbA1c or just A1c. This is a blood test which measures the average level of blood sugar (glucose) over the past 2 to 3 months.
HOMA-IR – Short for Homeostatic Model Assessment of Insulin Resistance, commonly referred to in medical literature. This is a method used to quantify insulin resistance and beta-cell function. It is calculated by taking the fasting glucose times fasting insulin divided by 405. (FG x FI/405) Desired range: 1.0 or lower. Over 2.5 is insulin resistance.
Type 1 Diabetes – (also known as Juvenile Diabetes, or insulin-dependent diabetes) When the body doesn’t produce enough insulin because its immune system is destroying the beta cells in the pancreas which is where insulin is made. The cause of Type 1 Diabetes is unknown.
Type 3 Diabetes – Not a medically recognized type of diabetes but an informal term for Alzheimer’s.
Oral Glucose Tolerance Test (OGTT) --. Common test used to diagnose diabetes and prediabetes by measuring the body's ability to use glucose. Involves fasting overnight, then the fasting blood sugar level is measured followed by consuming a sugary liquid drink and testing blood sugar levels periodically for the next two hours. This test has been debated within the ApoE4 forums for its comprehensiveness deferring to Dr Joseph Kraft’s test better accuracy in determining diabetes and prediabetes.
Dr Joseph Kraft – Referred to numerous times within the ApoE4 forums. Dr. Kraft’s test is similar to the oral glucose tolerance test (OGTT), but runs longer and adds insulin measurements. He found that 80% of those who had normal glucose responses had abnormal insulin responses. In other words, subjects who would be classified as “normal” under Fasting Glucose Tests, thereby not even progressing to an OGTT test, are not “normal” in their insulin response. For more info search see Dr Joseph Kraft or read his book "Diabetes Epidemic & You." Dr Catherine Crofts has also been referred to within the forums, she did her PhD work using Dr. Kraft's data. Discussions on both of these individuals can be found by using the advanced search function ApoE4.info Advanced Search Function..
Insulin Resistance’s link to Alzheimer’s and other Apoe4 health concerns
When an individual who has just learned their ApoE4 status comes to the ApoE4.info website, they are directed to the thread An introduction to ApoE4, biochemestry, and possible prevention strategies From this it says:
- Lowering insulin resistance. Many researchers and doctors, and many on our forum including myself, think this is the most important thing you can do to hopefully prevent AD. In addition, it is critical for prevention of CVD. This latter statement is not controversial at all. [italicized/bold emphasis added]
As many health issues have common roots originating from insulin resistance, this advice is good for all genetic populations, but especially for ApoE4s given the association with Alzheimer’s, cardiovascular disease, and lowered longevity.
Insulin Resistance's Link to Alzheimer’s disease
The term Type 3 Diabetes has remained popular since the 2008 article, Alzheimer's Disease is Type 3 Diabetes-Evidence Reviewed. The study concluded that, “the term “type 3 diabetes” accurately reflects the fact that AD represents a form of diabetes that selectively involves the brain and has molecular and biochemical features that overlap with both type 1 diabetes mellitus and T2DM.”
Since 2008, there has been much additional research, and the link between between Alzheimer’s disease (AD) and insulin resistance is even stronger. Some studies and their quotes:
- Insulin resistance and reduced brain glucose metabolism in the aetiology of Alzheimer’s disease published December 2016, http://insulinresistance.org/index.php/jir/article/view/15
- “Significant epidemiological and clinical evidence has emerged that suggests Alzheimer’s disease (AD) can be added to the list of chronic illnesses that are primarily caused by modern diets and lifestyles at odds with human physiology. High intakes of refined carbohydrates, insufficient physical activity, suboptimal sleep quantity and quality, and other factors that may contribute to insulin resistance combine to create a perfect storm of glycation and oxidative stress in the brain. Specific neurons lose the ability to metabolise and harness energy from glucose, ultimately resulting in neuronal degeneration and death. Simultaneously, chronic peripheral hyperinsulinaemia prevents ketogenesis, thus depriving struggling neurons of a highly efficient alternative fuel substrate.”
- “However, a diagnosis of T2D is not required for eventual progression to AD, because T2D does not cause AD. Rather, they may be thought of as ‘physiological cousins’ – conditions that result from the same underlying metabolic disturbances, but which have different outward manifestations in the body. One may be a diagnosed T2 diabetic and not develop AD, and many AD patients are not diagnosed diabetics.”
- “There is a significant link between Alzheimer’s disease and impaired fuel metabolism in the brain, with disturbed cerebral glucose metabolism being an invariant pathophysiological feature of AD.23 The defining metabolic signature of AD is a decrease in the cerebral metabolic rate of glucose (CMRglu). This may be the primary underlying cause of neuronal degeneration and death: at its heart, AD is an energy crisis in the brain. It is the death of neurons via starvation, as they have lost the capacity to effectively harvest energy from glucose.”
- “It is certain, however, that brain insulin dynamics play a role in neurotransmission, cognition, and the regulation of hormones that control feeding behaviour and reproductive function.32”
- “One potential aggravating factor for the ApoE4 genotype is that ApoE4 homozygotes produce 50% less hippocampal IDE compared to healthy controls, as well as AD patients who are not carriers of the ε4 allele.36”
- Unraveling Alzheimer's: Making Sense of the Relationship between Diabetes and Alzheimer's Disease published April 2016 https://www.ncbi.nlm.nih.gov/pubmed/26967215
- “Numerous studies have documented a strong association between diabetes and Alzheimer's disease (AD). The nature of the relationship, however, has remained a puzzle, in part because of seemingly incongruent findings.…However, careful integration of multiple strands of research, with attention to the methods used in different studies, makes it possible to disentangle the research on AD. This integration suggests that there is an important relationship between insulin, IDE, [Insulin Degrading Enzyme] and AD that yields multiple pathways to AD depending on the where deficiency or excess in the cycle occurs. I review evidence for each of these pathways here.”
- “Importantly, Cook et al. found that AD patients with the ApoE4 allele had a 50% reduction in expression of IDE compared to AD patients without the ApoE4 allele, suggesting that the ApoE4 allele may play a role in IDE deficiency leading to AD [95].”
- Epidemiology of dementia: the Hisayama study April 2014 https://www.ncbi.nlm.nih.gov/pubmed/24796086
- “In our prospective study, diabetes was associated with significantly increased risk of Alzheimer's disease and vascular dementia”
- Effects of Glucose and Insulin on Secretion of Amyloid-β by Human Adipose Tissue Cells published July 2016 https://www.ncbi.nlm.nih.gov/pubmed/27172814
- “Aβ was made by adipose tissue cells in vitro at concentrations similar to in vivo measure¬ments. Regulation of Aβ production by glucose and insulin and effects of Aβ on the insulin receptor path-way suggest similar cellular mechanisms may exist between neuronal dysfunction in Alzheimer disease and adipose dysfunction in type 2 diabetes.